Patients with a suspected type of liver disease that affects up to 30 per cent of Australians will take part in a $1 million Australian Government Medical Research Future Fund trial in four regional and one inner-city Queensland GP clinics.
- Non-alcoholic fatty liver disease affects up to 30 per cent of Australians and is associated with obesity and type 2 diabetes
- $1 million study will trial mobile clinics in regional centres to triage mild and severe cases of NAFLD
- The burden of liver disease costs Australia about $51 billion a year
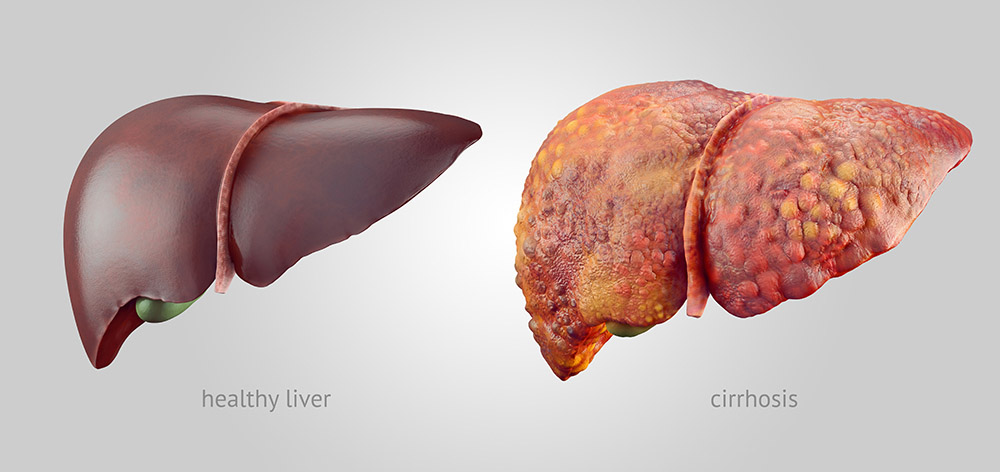
- Advanced NAFLD can lead to cirrhosis, liver cancer or liver failure

The trial aims to triage mild cases of non-alcoholic fatty liver disease (NAFLD) that can be managed locally by the GP, from advanced liver disease requiring specialist attention.
NAFLD is the most common type of chronic liver disease in Australia.
Study lead investigator Professor Adrian Barnett, from QUT’s Institute of Health and Biomedical Innovation, said the study would trial a better and faster assessment of 150 patients in regional areas, where obesity is at a higher rate, in association with their GP clinics.
“The condition is associated with obesity and type 2 diabetes and is likely to increase in the population as obesity rates rise,” Professor Barnett said.
“A mobile clinic with specially trained nurses will screen patients with abnormal liver function tests with a Fibroscan® that detects liver scarring.

“Currently people with abnormal liver tests are referred to hospital-based specialist clinics.
“They face a long wait for clinical assessment as to whether they are low-risk and can be managed with diet and exercise changes by their GP or at high-risk of complications such as cirrhosis (scarring of the liver), or liver cancer, and need specialised treatment.
“This would save all patients, especially regional people, time and money and take some of the burden off the hospital-based clinics.”
Princess Alexandra Hospital hepatologist and UQ researcher Professor Elizabeth Powell is a co-investigator on the study.
“NAFLD is common – 70-80 per cent of people with central obesity and 50-80 per cent of people with type 2 diabetes have this condition,” Professor Powell said.
“The cornerstone of NAFLD treatment is increased physical activity and healthy weight management – the same lifestyle habits that reduce the risk factors for cardiovascular disease and diabetes.
“Although fewer than 5 per cent of people with NAFLD develop clinically significant liver disease, its high prevalence means that the number of people with advanced liver disease is predicted to increase over the next decade, and NAFLD will likely become a leading indication for liver transplantation in Australia.”
Professor Powell said people with non-alcoholic fatty liver disease often had no symptoms, and the diagnosis usually followed the incidental finding of mildly abnormal liver tests or a fatty liver on abdominal ultrasound examination.
“The condition is often under-recognised by GPs, and so we hope this study will raise awareness of the prevalence of the condition and the importance of assessing the extent of liver scarring,” she said.
“If the subset of patients with NAFLD who have clinically significant liver disease are not detected, and liver scarring progresses untreated, it increases the risk of developing cirrhosis and complications of advanced liver disease such as liver cancer and liver failure.
“If everyone with non-alcoholic fatty liver disease were to be referred to a hospital-based liver clinic, it would overwhelm our health system.
“The Fibroscan® is a simple non-invasive tool that can help us assess the extent of liver scarring, and whether a patient may require referral to a liver clinic for further investigation and management. The results from this trial can potentially lead to better health and wellbeing for patients and save millions of healthcare dollars.”
The LOCATE trial begins in mid-2020 and will focus on the Sunshine Coast and Metro South regions.
Investigators:
QUT – Professor Adrian Barnett, Dr Sanjeewa Kularatna, Dr David Brain
University of the Sunshine Coast – Professor James O’Beirne
Metro South Hospital and Health Service – Dr Ingrid Hickman
University of Queensland – Professor Elizabeth Powell
QIMR Berghofer Medical Research Institute – Associate Professor Patricia Valery
QUT Media contact:
Niki Widdowson, 07 3138 2999 or n.widdowson@qut.edu.au
After hours: Rose Trapnell, 0407 585 901 or media@qut.edu.au.




